An Evidence-Led Case For Employer-Funded Flu And COVID Vaccination At Work
Are you thinking about offering workplace flu vaccinations but need colleagues to buy in? Or do you already run a flu programme and want to work out whether adding COVID vaccination is worth it?
Well, this guide should answer most of the questions that come up as you review your options.
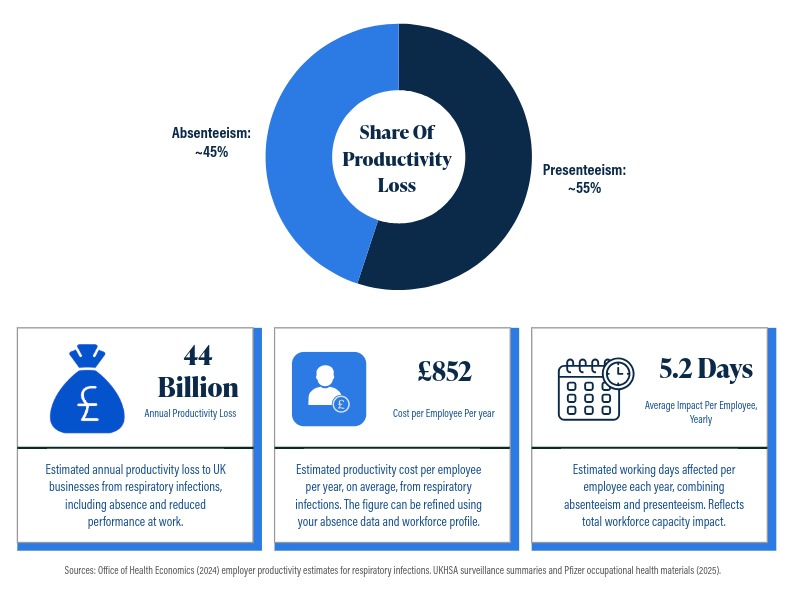
Respiratory infections are estimated to cost UK businesses around £44 billion each year in lost productivity (Office of Health Economics, 2024). A substantial share of that burden sits in presenteeism, the productivity loss that occurs when employees work while unwell and operate below their usual capacity (Pfizer, 2025a). Because presenteeism is less visible than recorded sickness absence, it is often under-measured and underweighted in senior funding decisions (CIPD, 2025a).
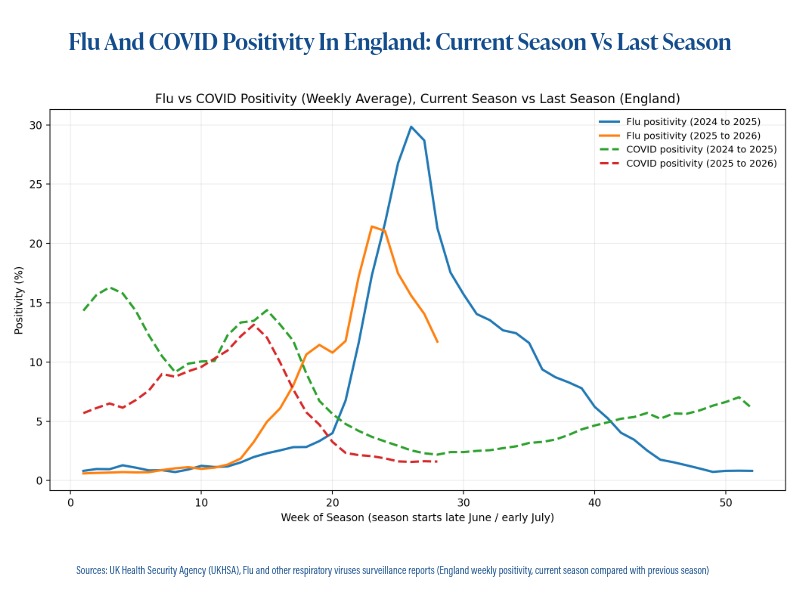
Workplace flu vaccination programmes are familiar because influenza follows a more predictable winter pattern, which supports clearer planning and justification (UKHSA, 2025a). COVID does not always follow the same seasonal rhythm and protection reduces over time, so disruption can occur outside the core flu window (UKHSA, 2025a; UKHSA, 2025b). When an employer vaccinates for flu only, they reduce one component of the respiratory burden but leave a meaningful share of productivity loss uncovered (Office of Health Economics, 2024).
This article sets out an evidence-led business case for offering flu and COVID vaccination together, using cost and workforce impact estimates and independent evidence that employees who repeatedly work while unwell are more likely to have future sickness absence and report worse overall health over time (Skagen and Collins, 2016).
Summary Statistics
Respiratory infections are estimated to cost UK businesses around £44 billion each year in lost productivity (Office of Health Economics, 2024).
Estimated employer cost is around £852 per employee per year (Office of Health Economics, 2024).
Estimated impact is around 5.2 days per employee per year, combining absenteeism and presenteeism (Pfizer, 2025a).
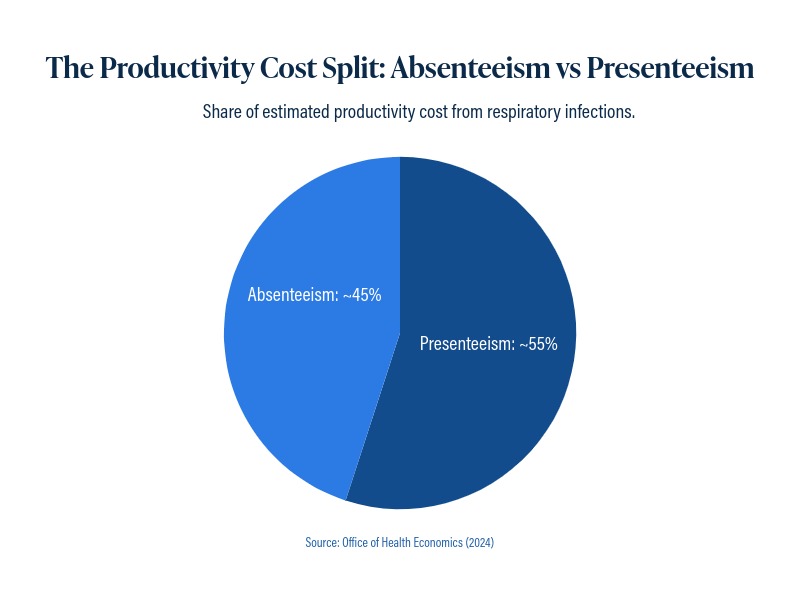
Presenteeism accounts for 54 to 55 percent of total productivity cost in the employer estimates (Office of Health Economics, 2024).
The employer survey results show that 66 percent of employees view employer-funded vaccination positively, and 80 percent of those say they would be likely to take it up (Pfizer, 2025a).
Table of Contents
Show
▾
Table of Contents
Show
▾
- Why Employers Often Combine Flu And COVID Clinics
- Vaccination As A Workplace Intervention
- Co-Administration And Operational Efficiency
- Demand And Uptake
- Delivery Models That Make Programmes Work
- How Employers Can Apply These Findings With Doctorcall
- Planning Timeline For Workplace Vaccination
- Evidence And Sources
- Reference List
Why This Topic Matters Now
Most organisations track sickness absence and use those figures in risk and budget discussions. Reduced performance while employees work through illness is measured far less consistently, including the growing pattern of working from home while unwell (CIPD, 2025a). This can lead to an underestimation of total productivity loss and an undervaluation of prevention measures.
In parallel, UKHSA surveillance continues to monitor influenza, COVID and other respiratory viruses across the year, drawing on community, primary care, secondary care and mortality data. For HR, occupational health and healthcare leaders, this ongoing surveillance supports a more realistic planning assumption that respiratory disruption is not confined to one narrow winter peak (UKHSA, 2025a).
When organisations measure absence but not at-work impairment, the case for prevention can look weaker on paper even when the operational impact is significant (CIPD, 2025a).
More than half of the productivity cost sits in presenteeism. If you only measure absence, you can understate the true business burden.
ROI Toolkit For Employer Decision Makers
This section provides a straightforward way to estimate the scale of respiratory-related productivity loss in your organisation and to compare what is covered by a flu-only programme versus a combined flu and COVID programme.
Repeatable Calculation
- Confirm employee count
Use your current headcount for the group you want to cover. - Apply an annual cost per employee
If you do not have an internal estimate, use £852 per employee per year (Office of Health Economics, 2024). - Convert into days impacted
Use 5.2 days per employee per year, split into 2.4 absence and 2.8 presenteeism days (Pfizer, 2025a).
Estimate The Cost of Respiratory Illness In Your Workplace
Type your employee count to estimate workdays affected and the estimated annual cost to the business.
Enter Number Of Employees
Enter a number to see results update instantly.
Results
Updates instantly
Indicative estimate for planning and comparison. Your actual cost may be higher or lower.
Assumptions Used In This Calculator
£852 per employee is used as the estimated annual productivity cost from respiratory illness (Office of Health Economics, 2024).
5.2 days per employee per year is used as the total workdays affected (Pfizer Ltd, 2025a, PP-UNP-GBR-11264, unpublished).
2.4 days absenteeism and 2.8 days presenteeism are used within the 5.2 days total (Pfizer Ltd, 2025a, PP-UNP-GBR-11264, unpublished).
Sources: Office of Health Economics (2024)
https://www.ohe.org/publications/employer-costs-respiratory-infections-survey-data-business-burden
Pfizer Ltd (2025a), Private UK Occupational Health Digital Leavepiece (PP-UNP-GBR-11264), unpublished.
Planning early helps secure preferred clinic dates in the core vaccination window.
How Senior Leaders Should Interpret The Result
The key insight is the split. A significant share of the burden is not sick leave. It is reduced performance when employees continue working while unwell. This is why absence figures alone can understate the true productivity impact of respiratory illness.
Flu-only vaccination reduces risk linked to influenza, but UKHSA surveillance shows COVID is circulating in the same season. In mid-October 2025, SARS-CoV-2 positivity in hospital PCR testing was 10.3%, while influenza positivity in lab surveillance was 6.1%, which shows why a flu-only programme can leave a meaningful share of respiratory infection uncovered. Adding COVID vaccination broadens coverage to more of the respiratory-related productivity exposure, including disruption outside the main flu period and where protection reduces over time. (UKHSA, 2025a; UKHSA, 2025b)
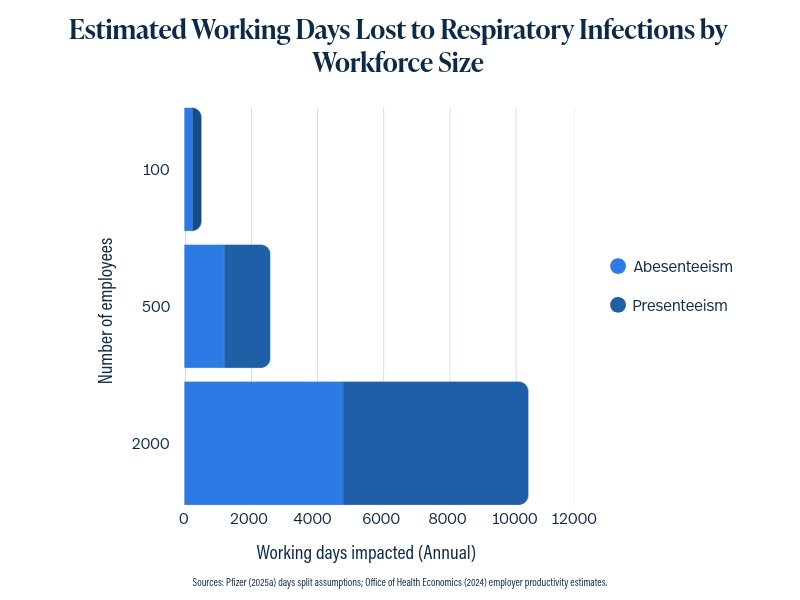
Worked Examples Using Standard Inputs
These examples illustrate scale and risk coverage. They do not claim a guaranteed saving.
| Workforce Size | Indicative Annual Productivity Exposure | Indicative Days Impacted |
|---|---|---|
| 100 employees | £85,200 | 520 days (240 absence, 280 presenteeism) |
| 500 employees | £426,000 | 2,600 days (1,200 absence, 1,400 presenteeism) |
| 2,000 employees | £1,704,000 | 10,400 days (4,800 absence, 5,600 presenteeism) |
Defining The Terms
Clear definitions matter because they shape what gets recorded, what gets reported and what receives investment. Absence is visible and routinely tracked. Sickness presenteeism is less visible, but it can account for a substantial share of the total productivity burden from respiratory infections (Office of Health Economics, 2024).
Absenteeism
Time away from work due to illness, typically captured through HR systems and therefore easier to quantify.
Presenteeism
Attending work while unwell when the health condition would reasonably justify taking sick leave, with reduced capacity and output (Society of Occupational Medicine, 2025).
The Operational Cost Of Working While Unwell
Many organisations measure the cost of winter illness through sickness absence and cover. That is only part of the impact. In roles that are hard to backfill, time-sensitive, safety-critical, or customer-facing, people often come in while unwell to avoid disruption. The cost then shows up as presenteeism, lower performance, more mistakes, slower output, and higher risk of spreading illness across teams. In many cases, that creates more absence later.
Schools And Education
Cover is hard to arrange and continuity matters, so staff may attend while unwell. When performance dips in a role that depends on attention and judgement, lessons run less smoothly, behaviour issues can rise, and planning and marking fall behind. Close contact also increases staff-to-staff transmission, which can worsen shortages later.
Healthcare And Care Settings
Services still need to run, even in peak demand. Staff may feel unable to stay away, which raises presenteeism risk. Small drops in attention and pace can affect throughput and decision quality across a shift, with added transmission risk to colleagues and clinically vulnerable patients.
Production Lines And Manufacturing
A single gap can slow an entire line and specialist roles may be difficult to cover. That pressure can lead to people working while unwell. The result can be bottlenecks, quality issues, more supervision, and higher safety risk where alertness matters.
Clean And Controlled Environments
In labs, cleanrooms, food production, and high-spec manufacturing, errors carry a high cost. People may still attend with mild symptoms, but fatigue and reduced concentration can increase deviations, rework, and in some settings, contamination risk that leads to costly interruptions.
Customer-Facing And High-Contact Sectors
In retail, hospitality, and transport, rotas are tight and short-notice cover is hard. People may work while unwell due to staffing pressure, pay, or not wanting to let the team down. Service slows, errors rise, customer experience drops, and illness spreads more easily through teams.
Across sectors, illness costs are not confined to recorded sick days. A significant share sits in reduced performance and onward transmission. That is why respiratory prevention plans should be assessed against total capacity impact, not absence alone.
The Real Cost Of Respiratory Infections For Employers
The estimates are useful because they translate respiratory illness into board-level measures. They present a national annual cost, a per-employee estimate and a framing in working days affected per employee each year.
Crucially, the same estimates split impact into absenteeism and presenteeism, with presenteeism accounting for 54 to 55 percent of the cost (Office of Health Economics, 2024). This matters because many organisations can quantify absence, but struggle to quantify at-work output loss.
Planning early helps secure preferred clinic dates in the core vaccination window.
Why Presenteeism Is The Hidden Cost
Presenteeism is often absent from standard reporting systems. Operationally, it can appear as slower throughput, more errors, lower service levels, longer decision cycles, higher pressure on colleagues and higher likelihood of onward transmission (CIPD, 2025a).
Independent evidence also suggests sickness presenteeism is associated with longer-term consequences, including later sickness absence and worse overall health over time (Skagen and Collins, 2016). This strengthens the business case for prevention because it links day-to-day underperformance with future capacity risk.
Flu Vaccination Is A Strong Foundation, Adding COVID Makes It Stronger
Workplace flu vaccination is a proven and practical intervention. Influenza activity in the UK typically peaks in late December, January or February and is not usually significant before mid-November (UKHSA, 2025c). That predictability is helpful for employers. It supports autumn planning and the aim of completing most vaccinations by the end of November, so protection is in place ahead of the winter peak (UKHSA, 2025d).
However, many employers now view flu cover as the baseline rather than the full answer. COVID is monitored alongside influenza in UKHSA surveillance reporting across the season, and disruption can occur outside the core flu window (UKHSA, 2025a). UK guidance also notes that protection wanes over time, particularly against symptomatic disease following boosters, which supports keeping timing and eligibility under review (UKHSA, 2025b).
For decision makers, the advantage is simple. Flu vaccination reduces a major seasonal risk. Adding COVID vaccination builds on that by widening the protection story to cover a broader share of respiratory disruption. It strengthens continuity planning by addressing both the predictable influenza peak and the additional risk that COVID can present outside that peak (UKHSA, 2025a; UKHSA, 2025b).
Why Employers Often Combine Flu And COVID Clinics
UKHSA surveillance reports monitor COVID circulation and other respiratory viruses across the season. The COVID Green Book chapter also notes waning protection over time, particularly for symptomatic disease after boosters, reinforcing the need for programme timing and eligibility to remain under review (UKHSA, 2025b).
For many employers, combining flu and COVID vaccination into a single clinic is also about operational simplicity. It reduces downtime from running multiple vaccination events across the year and makes it easier for employees to attend in one appointment (UKHSA, 2025a; UKHSA, 2025b).
Vaccination As A Workplace Intervention
Respiratory infection control is strongest when interventions reinforce each other. Ventilation, hygiene, staying home when unwell and vaccination each reduce risk through different mechanisms (UKHSA, 2023).
Vaccination supports business continuity because it can reduce infection risk and reduce severity where infection occurs, supporting both lower sickness absence and lower at-work performance loss.
Co-Administration And Operational Efficiency
Co-administration means giving the flu vaccine and the COVID vaccine during the same appointment, usually in different arms. For employers, the value is practical. A single visit reduces the time employees spend away from work, lowers drop-off between doses and avoids the disruption of running separate clinics.
UK guidance supports co-administration where it is operationally expedient (UKHSA, 2021).
Demand And Uptake
The employer materials suggest most employees respond well to vaccination when it is provided through work. In the survey findings, 66 percent viewed employer-funded vaccination positively. Among those, 80 percent said they would be likely to take it up (Pfizer, 2025a).
In practice, uptake is influenced by a small number of practical factors.
Convenience
On-site clinics, simple booking and options that fit shifts and hybrid working make it easier for people to attend. Voucher routes can also improve access for dispersed teams.
Trust and clear messaging
Uptake improves when communications are clinically grounded, consistent and easy to understand. Staff want to know what is being offered, why it matters and how to book.
Removing cost barriers
Employer-funded provision removes a common barrier, especially for lower-paid workforces.
How wording can increase uptake
Employers can also increase participation by using an opt-out style message that normalises attendance. For example, “Your vaccination has been reserved for you. Please choose a time” often performs better than “Would you like a vaccination?” because it frames vaccination as the default and reduces decision friction.
This approach works best when staff still have a clear choice, simple rescheduling options and a straightforward way to decline if they do not wish to take it up.
Delivery Models That Make Programmes Work
On-site clinics
Best for concentrated workforces with predictable attendance patterns and visible leadership support.
Pharmacy vouchers
Best for distributed workforces, shift patterns, higher turnover and hybrid working where attendance is less predictable.
Hybrid models
Best where organisations have multiple sites or mixed patterns and need to maximise coverage without unnecessary complexity.
How Employers Can Apply These Findings With Doctorcall
For organisations reviewing winter wellbeing and continuity plans, offering influenza and COVID vaccination through a single workplace programme can help address both recorded sickness absence and the less visible productivity loss linked to presenteeism.
In practice, value depends on delivery fit. On-site clinics can work well where employees are concentrated and attendance is predictable. Voucher routes can suit distributed teams, shift patterns, higher turnover and hybrid working arrangements. Many organisations use a combined approach to improve access across different employee groups. Planning early supports access to preferred clinic dates within the main vaccination window. Where required, egg-free flu options can be included within clinical planning.
For occupational health and benefits teams, the next step is usually a short scoping discussion based on workforce size, site footprint, working patterns, current flu arrangements, recent indicators of respiratory-related disruption and decision timelines. This supports a programme recommendation that is proportionate, operationally realistic and aligned with continuity priorities.
Planning Timeline For Workplace Vaccination
A month-based guide to keep planning in order and secure preferred clinic dates.
January to April
Build The Business Case
- Confirm objectives, absence, presenteeism, continuity cover.
- Define scope, flu only or flu and COVID.
- Map workforce, headcount, sites, shifts, remote or hybrid split.
- Pull internal indicators, trends, peak pressure, pinch points.
- Choose delivery model, on-site, vouchers, or mixed approach.
- Start supplier quotes and capacity checks.
- Begin due diligence, governance, consent, indemnity, cold chain, adverse events.
April to June
Budget Sign-Off And Supplier Selection
- Secure budget approval and named decision owners.
- Select supplier and confirm clinical lead and governance.
- Confirm vaccine types, including egg-free options if needed.
- Agree booking routes, consent flow, and reporting expectations.
- Lock preferred clinic date(s) with estimated numbers.
June to September
Engagement And Final Planning
- Run employee engagement to confirm demand and improve uptake.
- Confirm final numbers with the supplier.
- Finalise clinic format, slots and any walk-in capacity.
- Finalise logistics, rooms, privacy, queue plan, waste handling.
- Prepare comms support, manager briefing, FAQs, webinar if offered.
One Month Before Clinics
Execution Readiness
- Circulate booking link or appointment diary and reminders.
- Book room(s) and brief the site team involved.
- Confirm staffing ratios and on-the-day operational contact.
- Confirm escalation route, aftercare, and contingency cover.
During Clinics
Deliver And Monitor
- Monitor uptake and adjust access routes if needed.
- Capture simple metrics, attendance, issues and feedback.
After Clinics
Review And Secure Next Season
- Write a short outcome note, uptake, issues, lessons learned.
- Share feedback with the supplier and the business.
- Secure clinic date(s) early for next season.
Tip: Early booking helps secure preferred clinic dates within the core vaccination window.
Planning early helps secure preferred clinic dates in the core vaccination window.
Evidence And Sources
This article draws on two occupational health documents that synthesise three inputs.
- Employer interviews exploring what drives workplace vaccination uptake, barriers to uptake and what evidence is required to justify investment (Pfizer, 2025b).
- YouGov survey findings capturing employee sentiment and stated likelihood of uptake when vaccination is offered through employers (Pfizer, 2025b).
- Office of Health Economics estimates quantifying the productivity burden of respiratory infections and the distribution across absenteeism and presenteeism (Office of Health Economics, 2024).
The Office of Health Economics analysis referenced in the materials was commissioned and funded by Pfizer (Office of Health Economics, 2024). For balance, the argument uses independent sources on definitions and the downstream impacts of sickness presenteeism (Skagen and Collins, 2016; Society of Occupational Medicine, 2025).
Reference List
Show
CIPD (2025a) Health and wellbeing at work 2025. London: Chartered Institute of Personnel and Development. Available at
https://www.cipd.org/uk/knowledge/reports/health-wellbeing-work/
Office of Health Economics (2024) Employer costs from respiratory infections, survey data on the business burden. London: Office of Health Economics. Available at
https://www.ohe.org/publications/employer-costs-respiratory-infections-survey-data-business-burden
Pfizer Ltd (2025a) Private UK Occupational Health Digital Leavepiece. Internal occupational health communication material (PP-UNP-GBR-11264). Unpublished.
Pfizer Ltd (2025b) Private UK Occupational Health Decision Tool. Internal occupational health decision support material (PP-UNP-GBR-11265). Unpublished.
Skagen, K and Collins, A (2016) ‘The consequences of sickness presenteeism on health and wellbeing over time, a systematic review’, Social Science and Medicine, 161, pp. 169–177. Available at
https://pubmed.ncbi.nlm.nih.gov/27397729/
Society of Occupational Medicine (2025) Understanding sickness presenteeism, causes, risks and solutions. London: Society of Occupational Medicine. Available at
https://www.som.org.uk/understanding-sickness-presenteeism-causes-risks-and-solutions
UKHSA (2021) Vaccine update, issue 324, November 2021, flu special edition. London: UK Health Security Agency. Available at
https://www.gov.uk/government/publications/vaccine-update-issue-324-november-2021-flu-special-edition
UKHSA (2023) People with symptoms of a respiratory infection including COVID-19. London: UK Health Security Agency. Available at
https://www.gov.uk/guidance/people-with-symptoms-of-a-respiratory-infection-including-covid-19
UKHSA (2025a) Flu and other respiratory viruses surveillance reports. London: UK Health Security Agency. Available at
https://www.gov.uk/government/collections/flu-and-other-respiratory-viruses-surveillance-reports
UKHSA (2025b) COVID-19 the green book, chapter 14a. London: UK Health Security Agency. Available at
https://www.gov.uk/government/publications/covid-19-the-green-book-chapter-14a
UKHSA (2025c) Influenza the green book, chapter 19. London: UK Health Security Agency. Available at
https://www.gov.uk/government/publications/influenza-the-green-book-chapter-19
UKHSA (2025d) Annual flu programme. London: UK Health Security Agency. Available at
https://www.gov.uk/government/collections/annual-flu-programme
Office of Health Economics (2024) Employer costs from respiratory infections, survey data on the business burden. Figure used: presenteeism share of estimated productivity cost. Available at
https://www.ohe.org/publications/employer-costs-respiratory-infections-survey-data-business-burden
Calculator Using Your Organisation’s Figures
Enter your annual gross employment cost and headcount to estimate the annual cost exposure from respiratory-related illness.
Change any field to see the results update instantly.
Example shown as £10,000,000. Use department or whole-company employment cost.
Use the headcount covered by the programme.
Default is 230. This is based on 262 weekdays, less 8 public holidays and 24 leave days (262 − 8 − 24 = 230).
Results
Updates instantly
Indicative estimate for planning and comparison. It is not a guaranteed saving.
Notes And Sources
Calculations: Average gross employment cost per employee = total gross employment cost ÷ employees. Average daily employment cost per employee = average gross employment cost ÷ working days. Estimated annual cost to the business for respiratory-related illness = average daily employment cost × 5.2 days × employees.
Defaults used: 230 working days per year, based on 262 weekdays less 8 public holidays and 24 leave days (262 − 8 − 24 = 230). Days impacted per employee per year: 5.2 days, split into 2.4 absenteeism days and 2.8 presenteeism days. Source: Pfizer Ltd (2025a), Private UK Occupational Health Digital Leavepiece (PP-UNP-GBR-11264), unpublished.
